There is growing scientific interest in what is known as personalized medicine, a practice that makes it possible to identify differences between patients and adapt therapies to each case, improving the efficacy and results of treatments. Some examples of these medical applications include the use of advanced surgical models, or phantoms, to evaluate personalized surgeries without risk, and the development of scaffolds, or tissue engineering scaffolds specific to each patient that mimic natural tissues to support the healing and restoration of damaged tissues. However, the usefulness of these new therapies and their effectiveness in medical research are intrinsically linked to the fact that these models are able to accurately replicate the complexities of the tissues they intend to simulate or with which they must interact. Therefore, they have many advantages, but technologically there are many challenges in terms of reaching this stage of personalization. One of the main challenges is the limited availability of materials that can accurately mimic native tissues while capturing the complexity of their anatomy and shape.
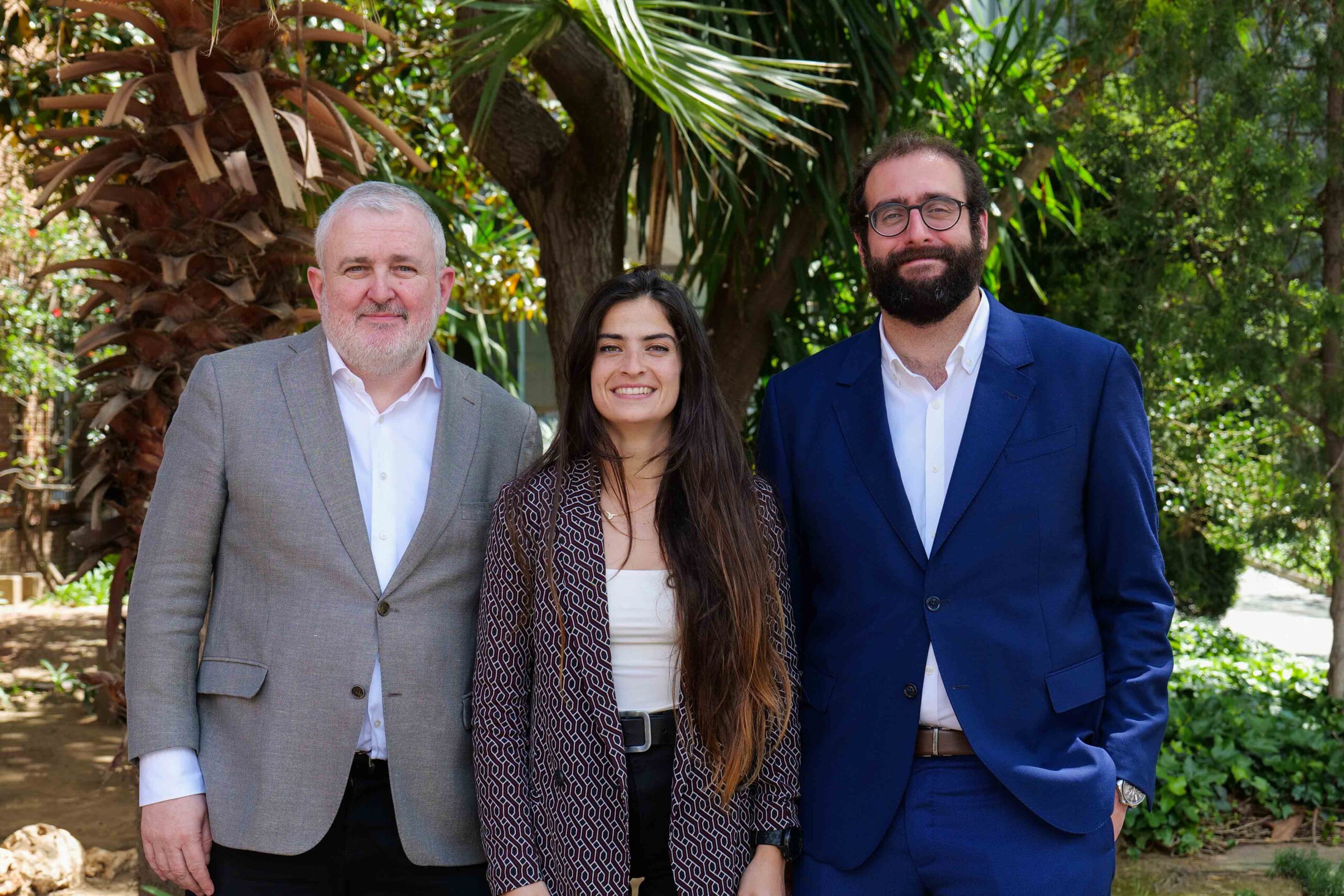
Within this context, and under the Materials Engineering Group (GEMAT) at the IQS School of Engineering, a research group with extensive experience in the development of new biomaterials for different applications, Dr Gloria Nieva Esteve has recently conducted her doctoral thesis entitled Exploring Biomimesis: integrating materials science strategies with 3D printing technologies to improve the replication of biological tissues. Her thesis was jointly supervised by Dr Salvador Borrós Gómez and Dr Robert Teixidó Bartés.
Dr Nieva focused her research on the development of materials that replicate biological tissues with different characteristics to improve their simulation and create them using advanced materials and technologies such as 3D printing.
Biomaterials serving regenerative medicine
Always from the perspective of what medical needs these challenges represent, Dr Nieva’s thesis focused on two very different aspects: recreating the biomechanical signalling of the tissues to be mimicked and, later, improving cell behaviour through the incorporation of substances of human origin into printing bioinks.
To achieve the first objective, materials based on silicone gels with adaptable viscoelastic properties were developed, which could improve soft tissue imitation and reproduce more realistic tissue and organ biomodels. Control of both the printing and viscoelastic properties of the materials was achieved by fine-tuning the silicone formulations using a rheology modifier and mechanical properties.
This new family of inks based on silicone gels facilitated the 3D printing reproduction of the different soft tissue profiles, which were validated in collaboration with the Sant Joan de Déu Hospital through an established medical protocol. In this first part of her thesis, Dr Nieva worked with the CIM Foundation at the UPC, developers of the 3D printer used, and obtained different kidney phantoms as a result of this collaboration.
The second objective of Dr Nieva’s research was to go one step further and develop bioinks, materials used for 3D printing scaffolds for tissue engineering, by incorporating biological materials extracted from human tissues. Overcoming the difficulties related to printing itself, structural integrity and biocompatibility, a family of bioinks was obtained with solid printing properties and structural stability over time under physiological conditions. Dr Nieva conducted this second part of her research in collaboration with the Blood and Tissue Bank (BST).
Her doctoral thesis represents an initial step in overcoming the great complexity of mimicking biological tissues, both from the point of view of simulation and substitution.
Related publication
Gloria Nieva Esteve et al., Developing tuneable viscoelastic silicone gel-based inks for precise 3D printing of clinical phantoms, Materials Advances, 2024, 5, 3706-3720. This thesis has been carried out within the framework of the BASE3D project, with the support of the Secretary of Universities and Research within the Government of Catalonia’s Department of Business and Knowledge, through the European Regional Development Fund (ERDF), and the QuirofAM project, cofinanced by ACCIÓ and the European Union through the European ERDF Fund.